
When many people think of an average lung cancer patient, they often imagine an older man smoking. But the face of lung cancer has changed. Over the past 15 years, more women, never smokers and younger people are being diagnosed with lung cancer.
In fact, lung cancer is the leading cause of cancer death among women, and more women die from lung cancer than breast, ovarian and colorectal cancer each year. The American Lung Association reports that while lung cancer rates have risen by 79% for women over the last 44 years, they decreased by 43% for men. And for the first time in history, there are more young women than men diagnosed with lung cancer.
As a thoracic oncologist at Sylvester Comprehensive Cancer Center, part of the University of Miami Health System, I have seen many younger women and never smokers walk into my clinic with a new diagnosis of lung cancer. Particularly for never smokers, lung cancer is unexpected for both patients and their doctors, which can often lead to delays in diagnosis. Researchers have described this trend of increasing lung cancer rates among women in different parts of the world and are starting to understand why cases are on the rise.
Lung cancer in women
The first explanation of why rates of lung cancer in women have increased is that many started smoking later than men, pushing back their peak in smoking-related lung cancer diagnoses.
Women also started smoking in the years when filtered cigarettes were most commonly used. This led to an increased risk of a type of cancer called adenocarcinoma due to the way cigarette filters distribute tobacco smoke to the outer parts of the lungs. Some studies suggest that women are more susceptible to the carcinogenic effects of exposure to tobacco and cigarette smoke, including second-hand smoke, and may develop lung cancer after fewer years of smoking compared to men.
However, it is important to note that most people diagnosed today with lung cancer are not active smokers. About 20% of women with lung cancer have never smoked – higher than for men with lung cancer who’ve never smoked.
Lung cancer risk factors
Besides smoking and secondhand smoke, there are several other lung cancer risk factors. These include a family history of cancer and exposure to asbestos, radon and air pollution.
Exposure to carcinogens in the workplace in the form of inhaled chemicals such as arsenic, beryllium, cadmium, silica and nickel is still a concern in some parts of the world. The potential lung cancer risk of e-cigarette and marijuana smoke is still under study but of potential concern.
Recently, researchers have also found that genetics can play a role in lung cancer risk in some patients with a strong history of lung cancer. Studies of these families have helped identify potential susceptibility genes for lung cancer and environmental risk factors.
Like BRCA1 and BRCA2 in breast cancer, alterations in genes that promote or protect against tumor development can contribute to lung cancer development. Researchers have yet to identify specific mutations that may predispose individuals to lung cancer. However, studying familial genetic predispositions can help elucidate how lung cancer develops and lead to new biomarkers for early cancer detection in high-risk groups.
Lung cancer screening
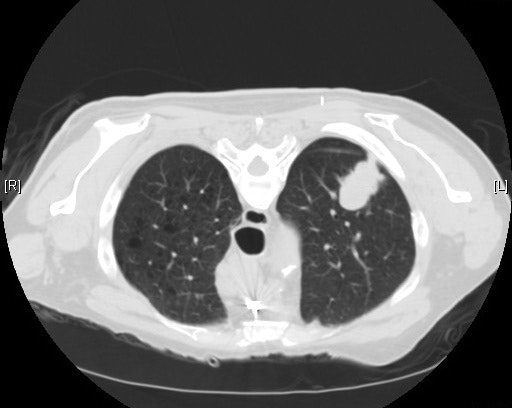
In 2021, the United States Preventive Services Task Force updated its lung cancer screening guidelines to include younger patients with less smoking history. Now, lung cancer screening is recommended for adults ages 50 to 80 who have smoked at least one pack per day for 20 years, current smokers and former smokers who quit smoking within the last 15 years. Women at risk for lung cancer can talk to their doctors about ordering a low-dose CT scan for lung cancer screening.
Nationwide, more than 70% of eligible women undergo breast cancer screening but less than 6% of all eligible smokers pursue lung cancer screening. Researchers estimate that these new screening guidelines will increase the number of women eligible for lung cancer screening by 40% by including those at a younger age who have less smoking exposure.
Lung cancer diagnosis
In recent years, increasing understanding of the genetic changes that can lead to cancer and how to harness the immune system to treat cancer has led to new targeted therapies and immunotherapies that have improved the prognosis of patients with lung cancer. Women tend to have a better lung cancer prognosis than men, especially if they never smoked and have tumors with molecular changes that can be treated with targeted therapies.
However, lung cancer symptoms may go unrecognized in women. Symptoms of lung cancer can include coughing, shortness of breath, overwhelming fatigue and pain in the back, chest or shoulder, which could be confused for other ailments. Because women tend to be slightly younger when diagnosed than men, patients may be able to tolerate symptoms longer and delay seeking medical attention. Physicians also might not attribute these symptoms to lung cancer due to a patient’s younger age.
Recognizing the early symptoms of lung cancer, expanding lung cancer screening eligibility and testing for genetic biomarkers to select the best therapy are some of the steps that could help address the global epidemic of lung cancer in women.
![]()
Estelamari Rodriguez is affiliated with University of Miami Health System. She receives funding from the American Cancer Society.