I cringed recently while driving to the clinic where I specialize in geriatric medicine when I heard a young radio announcer refer to old people as “wiggy,” a pejorative for wacky.
As a doctor who has extensively researched aging and age-related diseases for over 30 years, this to me is the sound of ageism unleashed.
The quip immediately underscored how easily society regards age as the sole measure of how well a person functions, rather than the person’s ability to think clearly, make decisions and perform daily tasks.
Aging and mental acuity
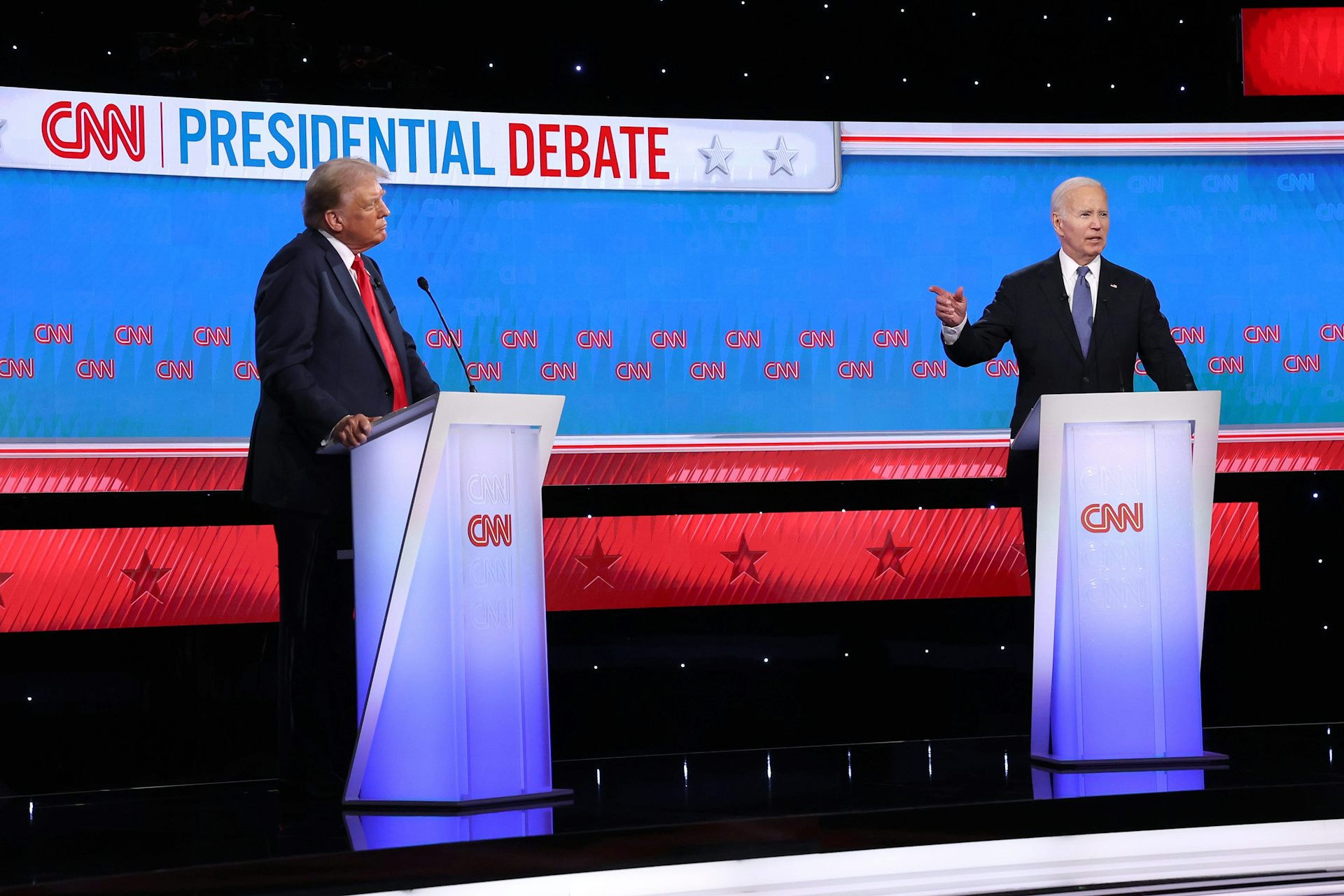
The tension between age and function certainly have played out on a world stage in the 2024 U.S. presidential campaign. Prior to President Joe Biden’s withdrawal from the election process in July 2024, a writer for a national magazine asked my expert opinion as to whether either or both presidential candidates exhibited signs of dementia.
My answer was that I could not make that kind of determination in the absence of neuropsychiatric testing, some laboratory tests and a comprehensive geriatric assessment. This evaluation measures the patient’s physical and mental health and assesses their ability to perform daily tasks and live independently.

The reporter then asked whether older people can be more susceptible to the effects of fatigue, stress and other psychological pressures that might be reflected in altered verbal performance.
My answer was yes, and I cited examples of how an aging brain under duress may lose a train of thought or engage in excessively long pauses or disconnected topics.
What’s more, our organs’ ability to self-regulate and maintain stability, known as homeostasis, declines as we age. In other words, our body does not bounce back from stressful situations as well as when we were young. For example, an older person may take two to three times longer to recover from jet lag than a middle-aged person.
The conundrum of the aging brain
While each organ ages at different rates, gerontologists can now estimate more accurately how a person’s biological age may differ from their chronological age. Biological age represents the physiological, biochemical or molecular profile that changes with age. The rate of this change may be slower or faster depending somewhat on genetics but mostly on lifestyle and environmental factors.
The results are often surprising. One 2021 study suggests nearly half of the 38-year-old participants were up to five years older in biological age than their actual age, while the other half were as many as five years younger.
But generally, in the absence of neurodegenerative disease, the aging brain works well. Research shows both good and not-so-good changes; the good changes include adaptations such as new learning strategies – such as using notes to augment memory.
Among the less desirable changes may be longer reaction time and reduced information processing – in other words, as we age, it may take longer to complete a task. Some older adults may also lose high-frequency hearing and miss some points in conversation, especially in a crowded environment.
But even most of those changes are subtle and really do not limit learning and executive function – that is, the ability to set and achieve goals, solve problems, regulate emotions and function normally overall.
Still, researchers are beginning to recognize a “no man’s land” between normal brain aging and late-life diseases of the brain. For example, periodic memory lapses may be recognized as mild cognitive impairment, which can represent a fork in the road, with half of these situations progressing to dementia and the other half either getting better or not worsening. Through adequate blood pressure control, regular exercise and cognitive engagement, many people show improvement.
Cognitive frailty
Physical frailty is characterized primarily by slowness, weakness and fatigue. But what’s now called “cognitive frailty” relates to increased sensitivity to stressors and less ability to bounce back from physical or mental stress.
Although cognitive frailty is not dementia, it is a potential precursor to dementia – when patients exhibit subtle but demonstrable cognitive changes.
This is an area that many clinicians, even those working in the field every day, do not fully understand. Many of them don’t dig deeply enough into those subtle changes expressed by older patients. Indeed, one study found that rural primary care doctors underrecognized dementia among their patients.
Primary care is lacking in sufficient screening for cognitive disorders. Furthermore, Medicare does not yet have a diagnostic code for cognitive frailty. That is why advocates for optimizing health care in older adults are promoting the routine use of the geriatric 4Ms in clinical practice for everyone 65 and older: medication, mentation, mobility and what matters. Mentation refers to the mind, while what matters has to do with what matters most to older adults.
This includes at least one annual screening for dementia and regular screening for the depression that can precede dementia.
Things you can do
Perhaps the most important question: What can all of us do to protect our brains and bodies from the negative effects of aging and disease as we get older?
Physical activity, cognitive stimulation and good blood pressure control are the key interventions for preventing the most common form of Alzheimer’s disease.
Research suggests that low-meat Mediterranean diets or Asian Indian diets, with spices such as turmeric, are buffers against brain aging. One emerging geriatrics concept is that slowing or reversing aging may circumvent dementia and other diseases. Current methods to slow aging include exercise and caloric restriction, or fasting. Yet others are looking toward oral supplements or alternative medicinals.
While old age itself should not be a factor for limiting people’s service to others, former presidents and senators have shown signs of cognitive impairment and frailty while in office.
The national discussion around President Biden and former president and presidential nominee Donald Trump’s mental acuity may be a catalyst to promote a larger conversation about aging, cognitive dysfunction and dementia, as well as what each of us can do to reduce our likelihood of developing cognitive problems late in life.
![]()
Donald Jurivich receives funding from HRSA (Geriatrics Workforce Enhancement Program).